People with neurogenic bladder and/or bowel dysfunction often suffer from highly individualized symptoms. It can be difficult to quantify change in an individual’s symptoms using standardized measurement tools, and points to the value of Patient—Centered Outcome Measures.
Read MoreTopics: Neurogenic bladder, Neurogenic bowel, Bowel dysfunction, Bladder dysfunction, quality of life
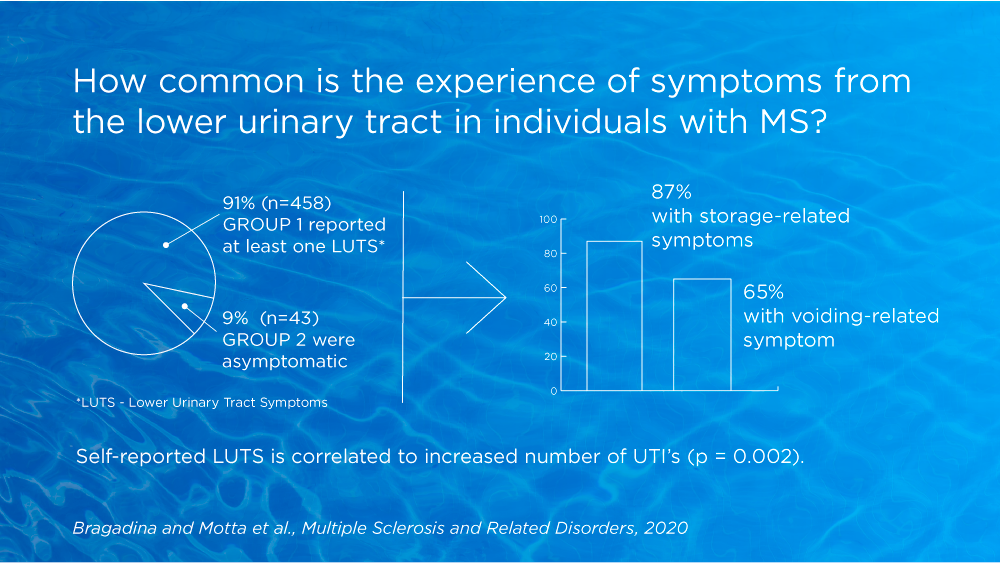
Storage and voiding symptoms often coexist, affecting up to 59% of individuals with MS. These clinical manifestations impact quality of life and are often associated with depressive symptoms, loss of work productivity, poor sleep quality and, in general, a deterioration in overall health. Problems related to micturition impede many people with MS from fully participating with family, friends and the community.
Read MoreTopics: Neurogenic bladder, Lower Urinary Tract Symptoms (LUTS), Bladder dysfunction, Multiple Sklerose (MS)
Information about the urinary microbiota is likely to modify the diagnosis, prevention and treatment of urinary disorders. This review highlights the role of urinary microbiota in development of several lower urinary tract (LUT) functional disorders.
Read MoreTopics: Bladder management, Bladder dysfunction, Lower Urinary Tract Symptoms
Prior to the LoFric Elle webinar in September, we had a great opportunity to talk to Susanne Vahr Lauridsen about the barriers related to intermittent catheterization and dignity. We also asked for her opinion on LoFric Elle’s potential to provide new opportunities for women facing challenges when performing IC.
Read MoreTopics: Neurogenic bladder, Bladder dysfunction, dignity, Lofric Elle
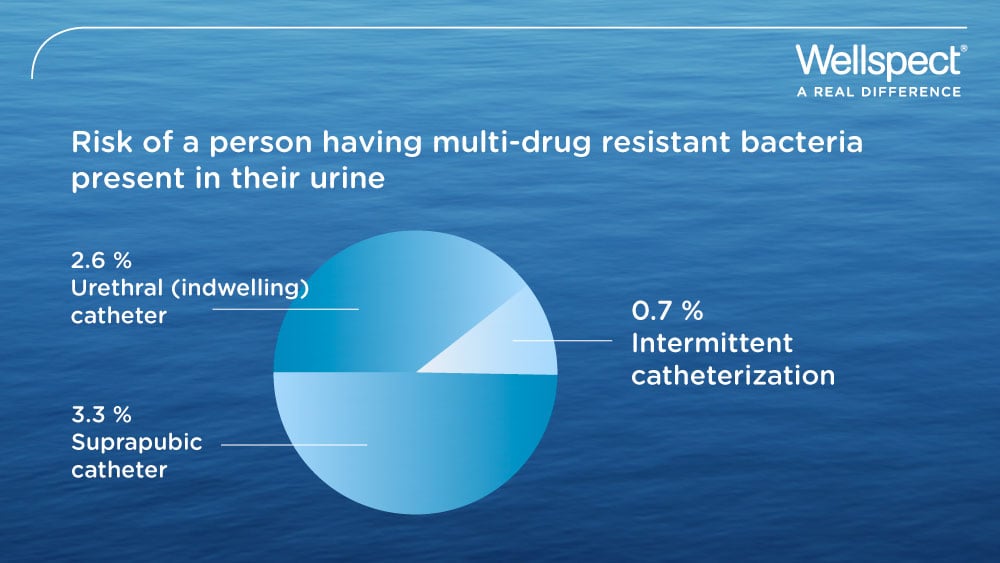
Patients with acute urinary retention are commonly given an indwelling catheter, thereby increasing risk of infection when compared to intermittent catheterization. A hospital in UK changed its practice and now uses self-catheterization as first-line management for patients presenting with acute urinary retention at the emergency department.
Read MoreTopics: Urinary Tract Infection (UTI), Catheter-associated UTI (CAUTI), Bladder dysfunction, Intermittent Catheterization