Studies on intermittent catheterization (IC) with larger samples sizes are rare and this study provides real-world evidence on IC use, which may be used to derive recommendations for improvement of care. This is among the first publications of a 3-year observation period including time before and after initial IC.
Studies on intermittent catheterization (IC) with large samples sizes are rare and this study is among the first to study a 3-year observation period including time before and after initiating IC. It provides real-world evidence on IC use, which may be used to derive recommendations for improvement of care.
Approximately 90% of the German population is insured in statutory health insurances, hence these sources of data are highly representative of the care reality in Germany. It’s a well-established procedure in health care research and internationally recognized, and this study provides directional insights to the economic burden within the healthcare system.
This descriptive study was conducted using the InGef research database from the German statutory health insurance claims data system. Individuals who initiated IC during 2013–2015 were included. The most common IC indications were urologic diseases, spinal cord injury, Multiple Sclerosis and Spina Bifida.
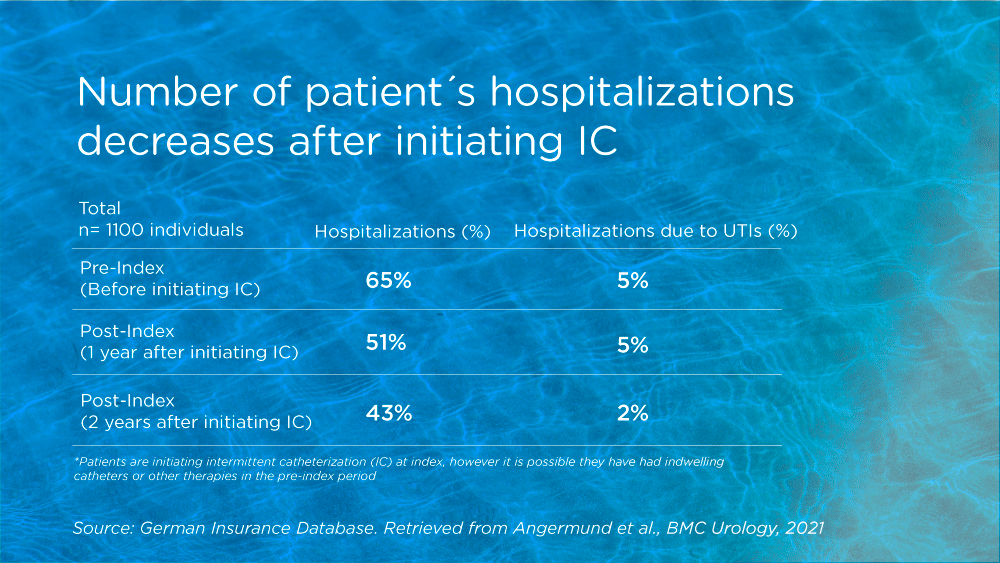
Urinary tract infections (UTI) were the most frequent complication, and in 61% it was shown to occur already in the year before starting with IC. Looking at follow-up data, 2-years after initiating IC, it actually decreased to 50%. Interestingly, data referring to hospitalizations and length of stay in hospitals as well as prescriptions of antibiotics, the highest numbers were shown before the individuals started with IC. This was true also for comorbidities, complications, and healthcare resource use. Follow-up data showed a decrease for these parameters from first to second year after initiating IC therapy.
Thus, the current data demonstrated that IC users experienced UTIs and high healthcare utilization and a potential high burden of illness already prior to initial IC. Regarding UTIs they were shown to decrease over time, suggesting that IC use has a positive influence on reducing infections and burden of illness. To mitigate health care costs and further support better outcomes, IC users should have continued access to products and therapies that best meet their unique bladder management needs. The findings from the current register data also showed that after a peak in the initial year of catheterization, healthcare costs decreased again in the second year of follow-up.




