Intermittent catheterization (IC) is frequently used to manage lower urinary tract dysfunctions, but research shows that care for patients using IC may not always be based on evidence. The purpose of this review was to summarize evidence related to adherence to IC, complication rates, satisfaction with IC, and its effect on health-related quality of life.
Urinary catheters have been used for more than 3500 years to drain the bladder when it fails to empty. Intermittent catheterization (IC) mimics normal bladder function and is considered the golden standard. In a recent cross-sectional study of 210 nurses based in the United States who regularly teach IC as part of their daily practice, it was found that almost two thirds (66%) do not base their practice on clinical guidelines. This supported the need for a summary of currently available evidence for this important nurse-led intervention.
Engberg and co-workers screened available literature among the four main databases for relevant articles and have summarized their findings in this review. The focus areas were:
- Ability to self-catheterize
- Adherence to the therapy
- Satisfaction and effect on health-related quality of life (QoL)
- Development of complications related to the therapy such as urinary tract infections, strictures and hematuria
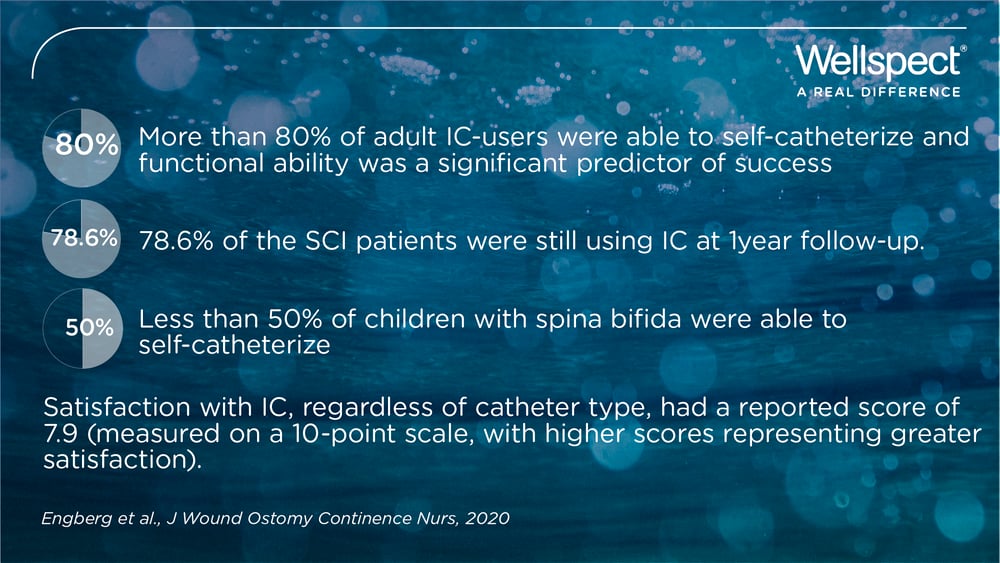
Results show that most patients can successfully perform IC and that functional status is likely the most important predictor of success. In studies on adults more than 80% of participants were able to self-catheterize. Numbers from a large study in the US on spinal cord injured patients showed that 78.6% of the patients continued using IC at 1-year following injury and rehabilitation. Often a higher percentage of men than women were adherent 6 weeks after being taught to perform IC.
Quality of Life (QoL) were measured in many different ways throughout the studies which makes it difficult to compare. The authors of this review conclude the following parameters to predict poor bladder-specific QoL in patients using IC:
- urinary incontinence
- UTIs
- pain during catheter insertion
- the need for a caregiver to perform the IC and poorer adherence to IC
Prophylactic antibiotic therapy may reduce the risk of recurrent UTIs and weekly cyclic antibiotic therapy (WCA) was reported to significantly reduce the rate of UTIs in 2 studies. WCA is a relatively new approach to preventing recurrent UTIs currently undergoing investigation. Prophylactic antibiotic therapy needs further investigation to confirm the results and should be carefully weight against the emerging problem with antibiotic resistance.
Yet, few studies are done to examine the link between UTI’s and constipation. A recent study in children supports the importance of bowel management by showing the rate of UTIs decreasing significantly more in the group treated with medication plus bowel management compared to only medication. The children who suffered from a mean of more than 3 UTIs per year reported less than 1 UTI the following year after the treatment.
The review by Engberg et al., 2020 also revealed multiple gaps in the evidence to support care for patients using IC. They like to see more research focusing on questions like suspected risk or protection factor(s) for IC-related complications as well as studies to determine how to improve outcomes for patients using IC to manage bladder function.




