We were happy for the engagement from our audience during the last of our three ACCT Let’s talk… webinars – this time with a focus on the Self and how to handle the delicate subject of intimacy and sexuality when somehow impaired. In fact, in answer to our question, 74% of our audience thought that the main barrier to seeking help for sexual dysfunction is embarrassment or the perceived taboo surrounding the subject. Which is why we think we need to talk about it.

During the live Q&A-session, our invited experts Professor Anton Emmanuel, Dr. Jalesh Panicker and Specialist nurse Collette Haslam brought great insights by answering questions from the audience but didn’t have time to reply to them all. Therefore, please find some more of their answers to selected questions below.
Professor Anton Emmanuel was asked why it’s so important to treat constipation – to which he replied as follows:
Constipation underlies many other presentations in neurogenic patients – reflux, abdominal pain, bloating, early satiety, limb spasms. So, improving constipation symptoms may improve several other presentations. Secondly, constipation leads to a major impairment of quality of life and dependence on carers. So, improving this symptom can also have a significant impact on people’s sense of wellbeing.
Then Professor Anton Emmanuel was asked to elaborate a bit on why the treatment pathways or algorithms are different between patients with functional and neurogenic bowel dysfunction even if the symptoms are the same?
He answered that the pathways are better developed since there have been more studies in functional bowel disorders (FBD). As more work is done in neurogenic bowel dysfunction (NBD), the path will become more complete. Also, in NBD patients the lack of sensation in some of them means that some of the laxatives (in particular osmotics and some prokinetics) can cause incontinence.
Bowel dysfunction is known to cause a substantial impact on quality of life, but which symptom has the most impact? This question was asked to the audience, and they replied as seen in the graph below:
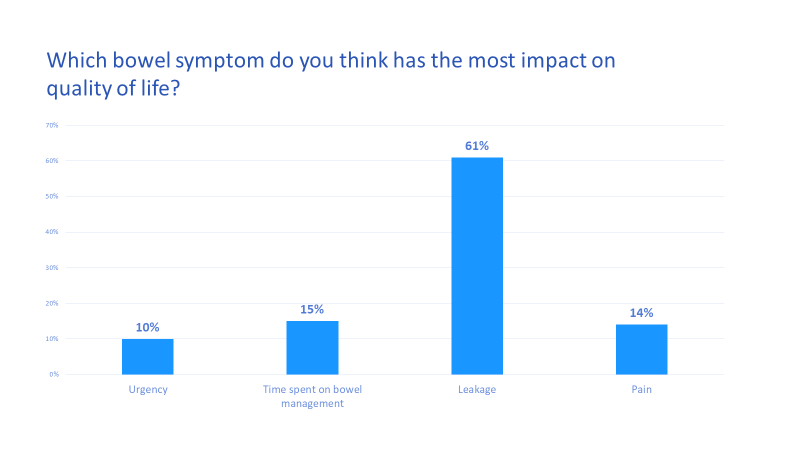
In other words, leakage is the symptom that is considered to have most impact on quality of life, which is well in line with the results from clinical studies.
The audience was curious to know whether Dr. Jalesh Panicker had experience or feedback when it comes to male patients on the benefit of the non-medication management such as touching, mapping, mindfulness etc.
Dr. Jalesh Panicker replied that we tend to focus on mechanical aspects of sexual dysfunction in males, but in those with severe numbness, the benefits of this non-drug management are poorly described. We don't know the long-term effects of interventions such as sensate focusing.
Are there any quality of life studies that show cost-efficiency in "restoring" sexual function in Neurological patients, was another question. Dr. Jalesh Panicker declared that there are published studies that demonstrate benefits of non-medical options for managing sexual difficulties in men, however the experience in his department has been limited to women with neurological disorders.
Most of the studies evaluating medications (phosphodiesterase 5 inhibitors) for neurogenic erectile dysfunction incorporate quality of life measures of great interest. However, studies that show cost-efficiency in "restoring" sexual function in neurological patients has not been explored.
Specialist nurse Collette Haslam was asked to explain whether treatment of bladder and bowel dysfunction improves sexual function. Upon which she told us that there are some studies to show that the use of treatment options such as Botox injections, percutaneous nerve stimulation and pelvic floor exercises can improve sexual function. This would be backed up by her personal patient reporting.
A follow-up question to this was whether she sees in her profession that treatment of constipation increases the ability to get an erection for some of the patients?
She described that in her experience she certainly sees co-morbidities between constipation and erectile dysfunction, physiological or psychological, she therefore insists that asking about bowel function should be included in all sexual function assessments.
Did you miss this webinar or any of the previous ones in the series? You can watch them on
demand here:




